Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

Powell in Jackson Hole
Jerome Powell delivers a key speech in Jackson Hole. Read the transcript here.

Trump Meets with Zelenskyy
Donald Trump participates in a bilateral meeting with Volodymyr Zelenskyy. Read the transcript here.
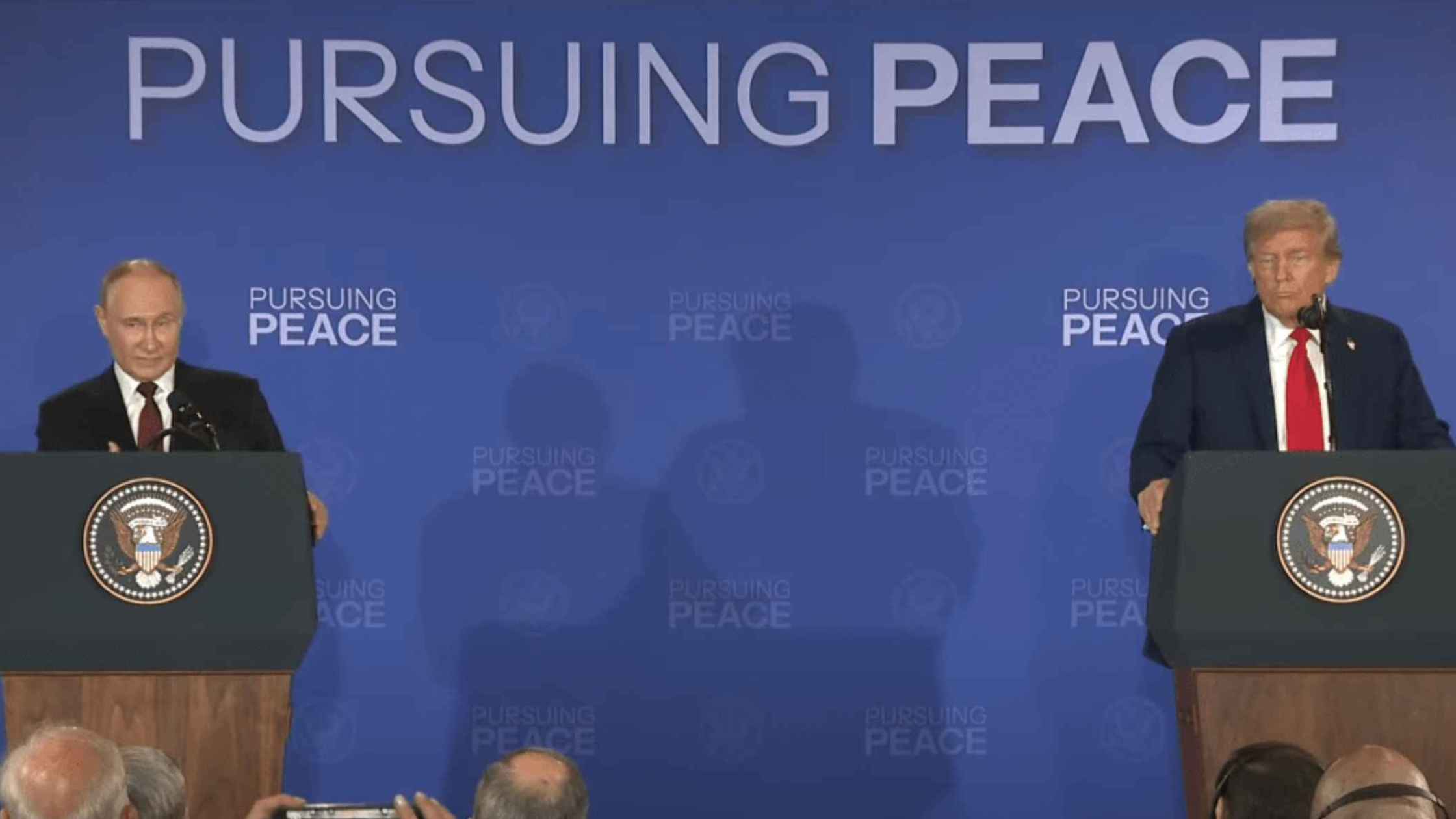
Trump and Putin Press Conference
Donald Trump Participates in a Press Conference with Vladimir Putin in Alaska. Read the transcript here.

Karoline Leavitt White House Press Briefing on 8/19/25
Karoline Leavitt holds the White House Press Briefing for 8/19/25. Read the transcript here.
DOJ Interview With Ghislaine Maxwell Day 1
Deputy Attorney General Todd Blanche of the DOJ interviews Ghislaine Maxwell day 1. Read the transcript here.
DOJ Interview With Ghislaine Maxwell Day 2
Deputy Attorney General Todd Blanche of the DOJ interviews Ghislaine Maxwell day 2. Read the transcript here.
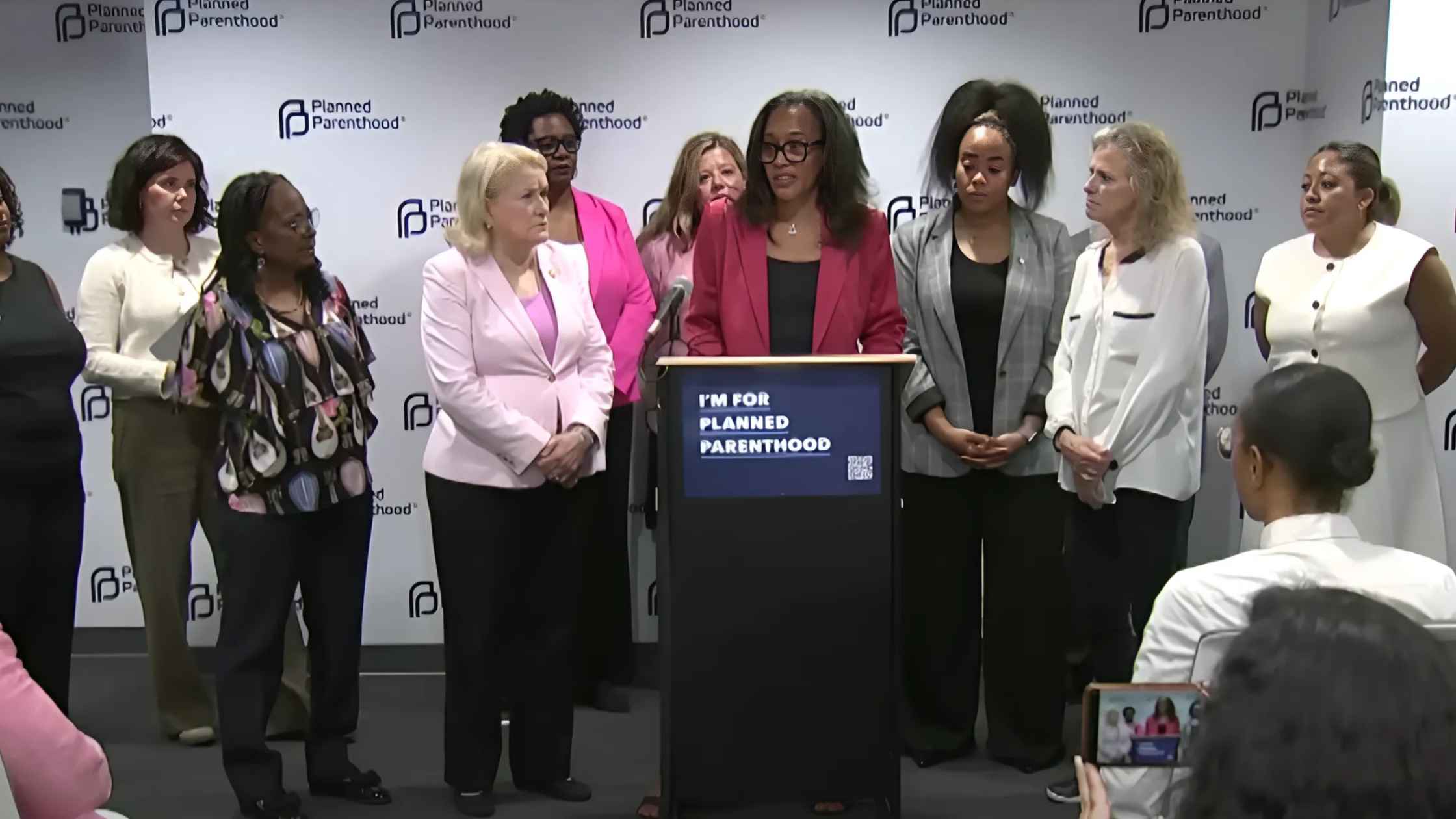
Texas Women's Healthcare Press Briefing
Texas Democrats hold news briefing on Planned Parenthood and women's healthcare. Read the transcript here.
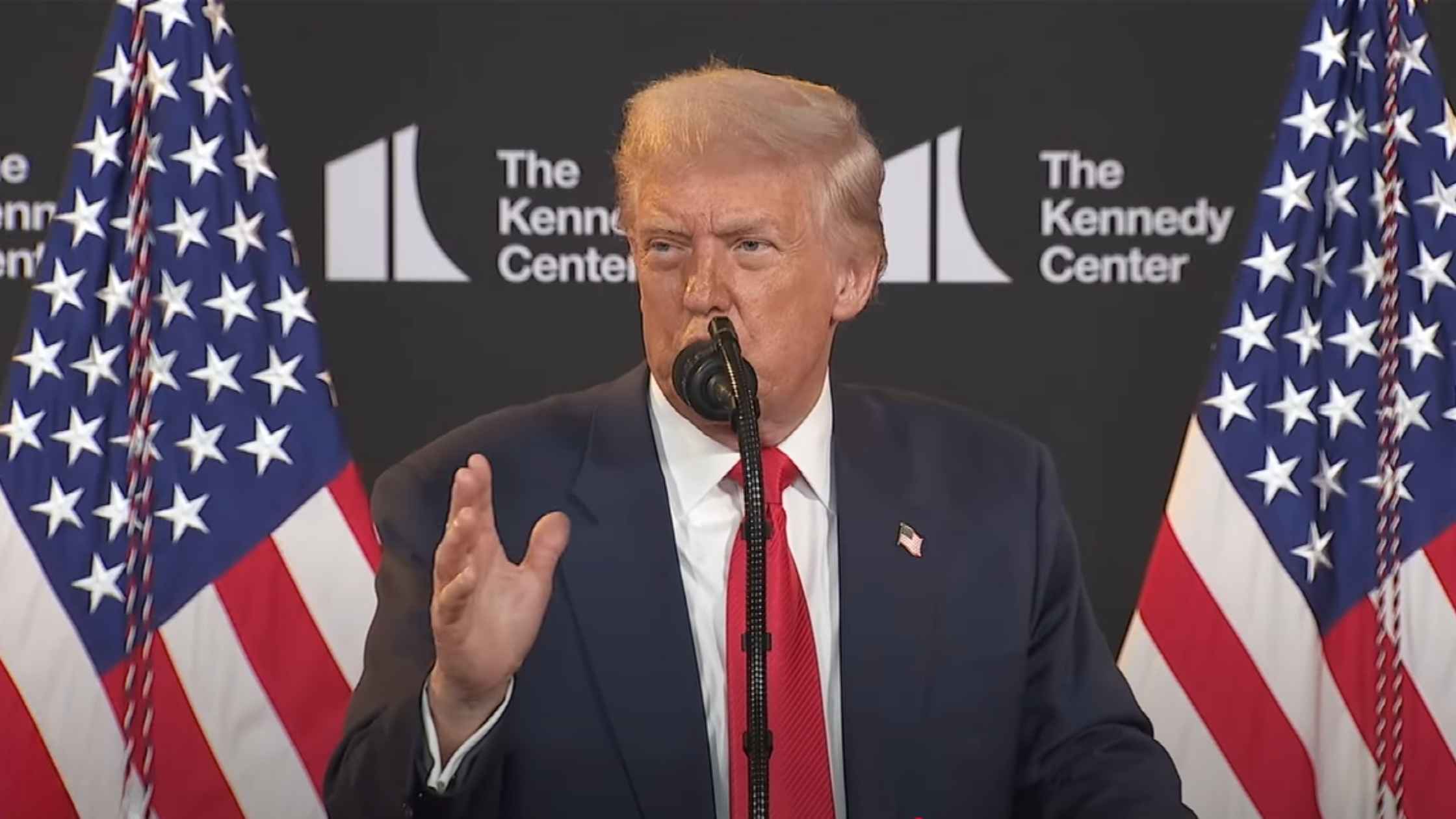
Trump Visits Kennedy Center
Donald Trump visits the Kennedy Center and announces new honorees. Read the transcript here.
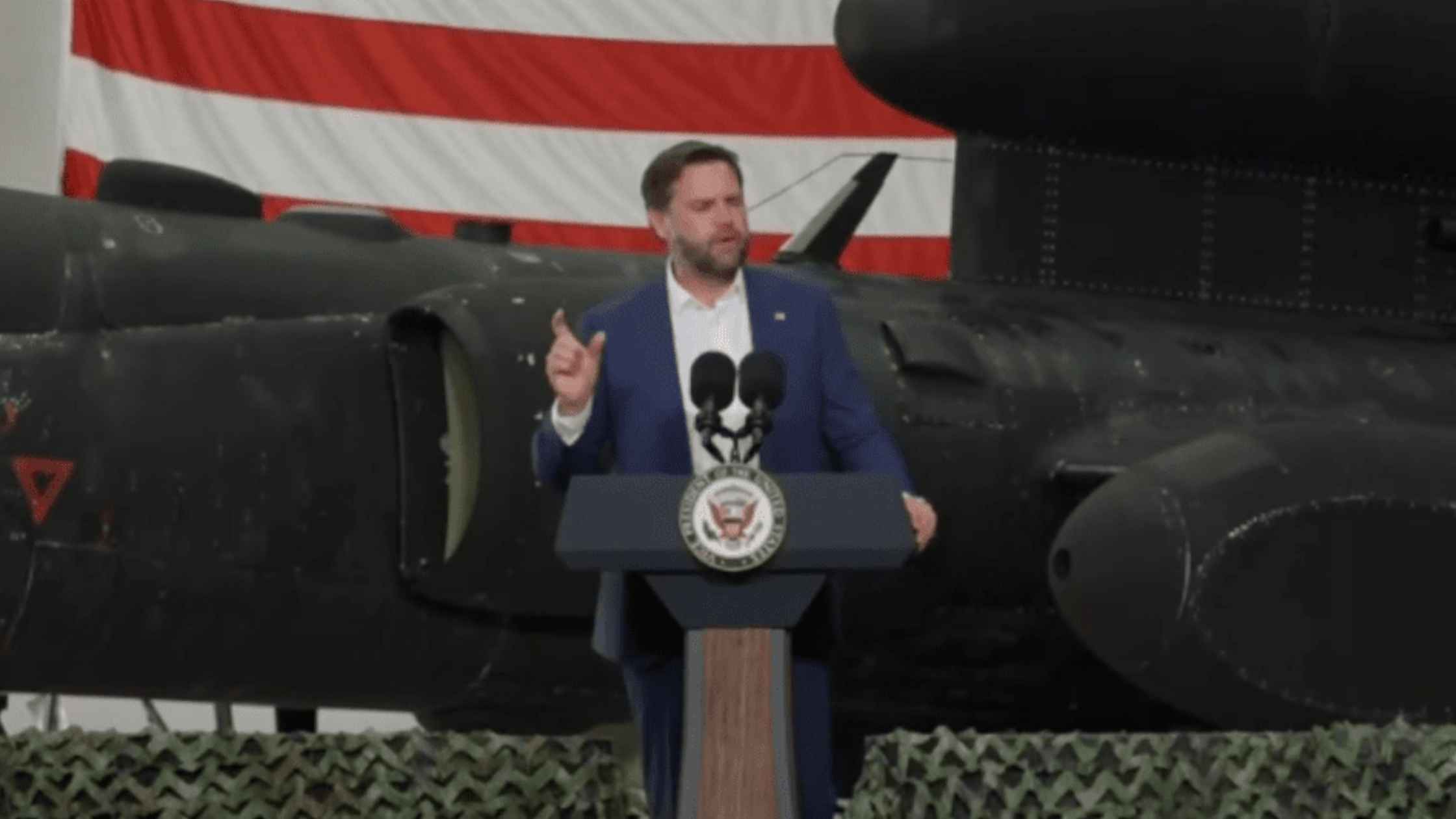
Vance at Royal Air Force Base
Vice President JD Vance visits with U.S. troops at Royal Air Force Base Fairford, England. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.

.webp)